What is Suboxone? Uses, Dosage and Misconceptions

This is where Suboxone can help. Suboxone is a medication that combines two ingredients—buprenorphine and naloxone—which work together to reduce cravings and ease withdrawal. It also helps prevent misuse by blocking the effects of other opioids. Studies show that Suboxone can lower the risk of fatal overdoses by 38 to 59%, making it an important part of addiction treatment.
Read on to learn more about how Suboxone works and to clear up common misconceptions about its use. Understanding Suboxone can help guide you or a loved one on the path to recovery.
What is Suboxone?
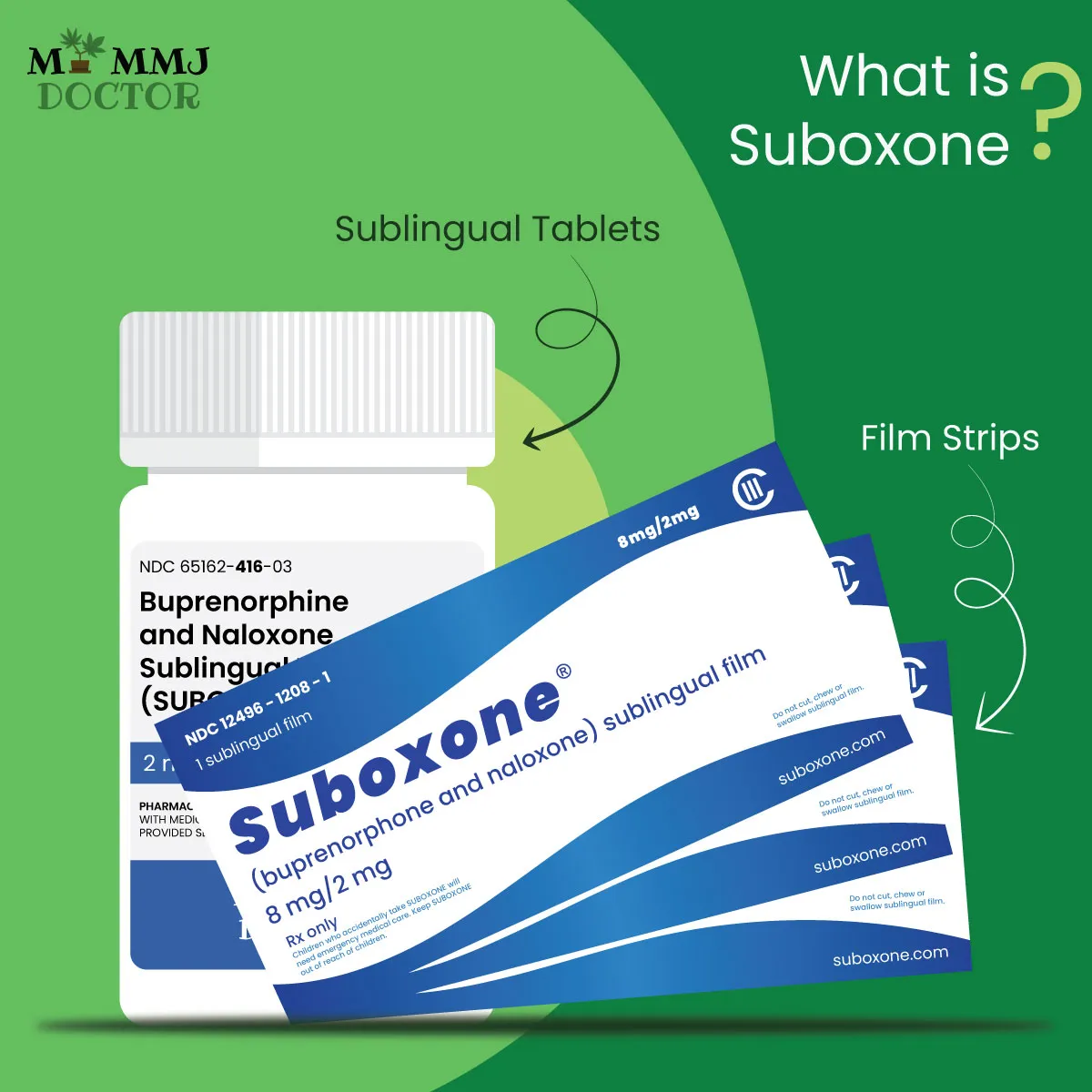
- Sublingual Tablets: These are placed under the tongue.
- Sublingual Film Strips: Also placed under the tongue, these dissolve quickly.
- Buccal Film Strips: These are placed between the gums and cheek.
All these forms dissolve rapidly in the mouth, similar to breath mint strips like Listerine. Suboxone comes in four strengths, ranging from 2 mg to 12 mg of buprenorphine.
The starting dose of Suboxone depends on the severity of the opioid addiction and is gradually reduced over time to help patients taper off the medication safely. The ultimate goal is to stop using Suboxone completely, with a carefully monitored process to minimize withdrawal symptoms. Patients often receive additional support through counseling and therapy to enhance their recovery.
What is the Right Dosage of Suboxone?
The dosage of Suboxone your doctor prescribes will depend on factors such as:
- The type and severity of your opioid dependence
- The stage of treatment you’re in
- Any other medical conditions you may have
Your doctor will usually start with a low dose and adjust it as needed to find the right amount for you. They will aim to prescribe the smallest effective dose.
Suboxone forms and strengths: Suboxone comes as an oral film placed under the tongue (sublingual) or in the cheek (buccal), available in these strengths:
- 2 mg buprenorphine / 0.5 mg naloxone
- 4 mg buprenorphine / 1 mg naloxone
- 8 mg buprenorphine / 2 mg naloxone
- 12 mg buprenorphine / 3 mg naloxone
Generic versions also come as sublingual films or tablets.
How Does Suboxone Work?
Suboxone is a medication used to treat opioid use disorder. It contains two main ingredients: buprenorphine and naloxone. Here’s how it works in the brain:
- Easing Withdrawal Symptoms: When you take Suboxone, it helps ease withdrawal symptoms that occur when someone stops using other opioids. This is because buprenorphine, one of its components, attaches to the same receptors in the brain as other opioids.
- Brain Chemistry: In your brain, there are special sites called opioid receptors. When opioids attach to these receptors, they can block the release of a neurotransmitter called noradrenaline, leading to feelings of drowsiness and pain relief. This process also causes the release of dopamine, which creates feelings of pleasure and reward.
- Partial Agonist: Buprenorphine is a “partial agonist,” meaning it activates opioid receptors but not as strongly as full opioids like heroin or fentanyl. This makes it effective in reducing cravings and withdrawal symptoms without producing the intense euphoria associated with other opioids.
- Naloxone’s Role: The naloxone in Suboxone helps prevent misuse. If someone tries to inject or snort Suboxone to get high, naloxone will block the effects of other opioids and can lead to immediate withdrawal symptoms, discouraging misuse.
How Suboxone Fits into Treatment?
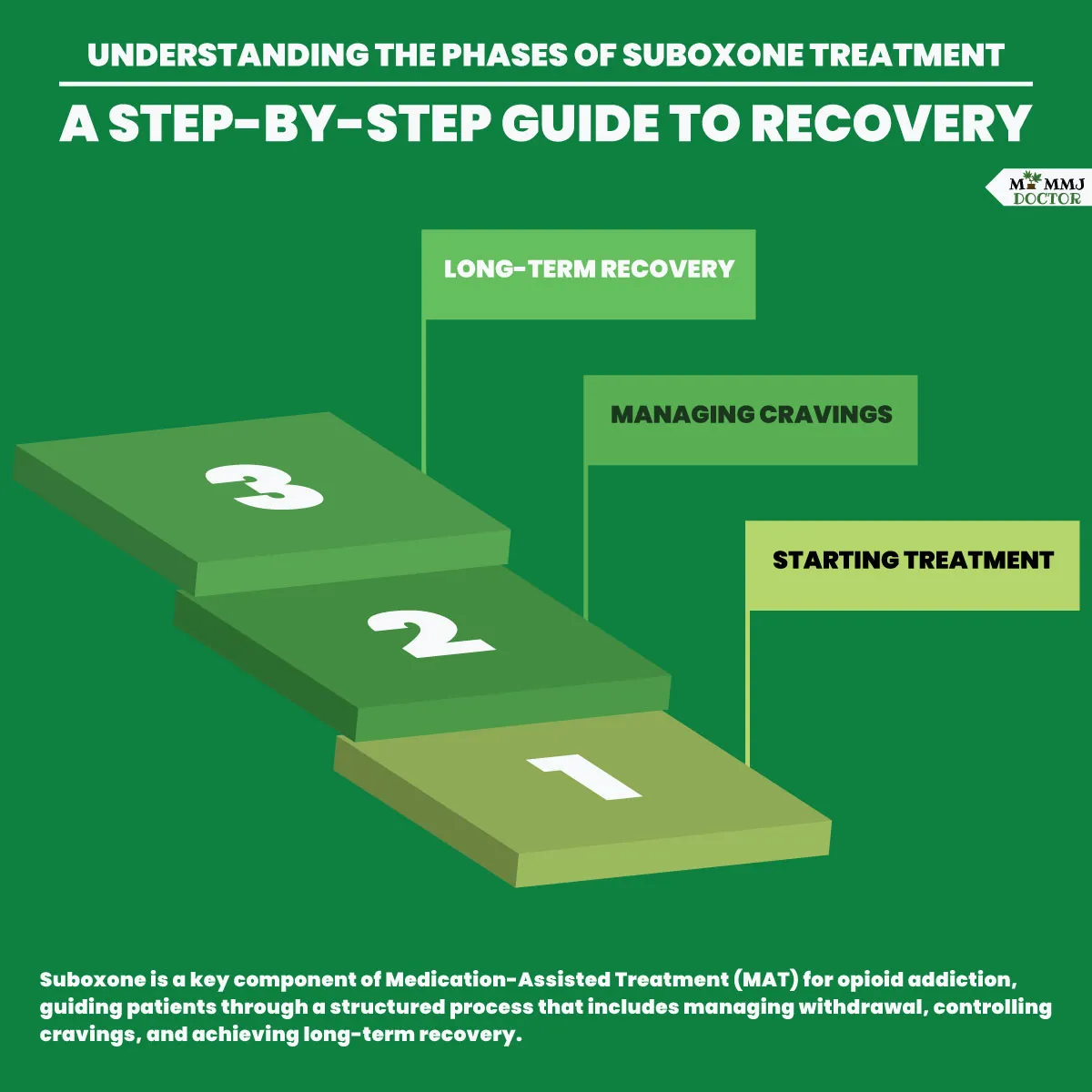
Phase One – Starting Treatment:
You meet with a healthcare provider who will review your medical history and create a treatment plan. They’ll monitor your withdrawal symptoms and adjust your Suboxone dosage to manage them.
Phase Two – Managing Cravings:
After withdrawal, your provider will check how well Suboxone is controlling your cravings and adjust the dose if needed. You’ll also attend counseling or therapy to build healthy coping skills.
Phase Three – Long-Term Recovery:
Once you’ve maintained sobriety for several months or more, your provider may start reducing your Suboxone dose. In some cases, you might stay on Suboxone long-term to keep you on track.
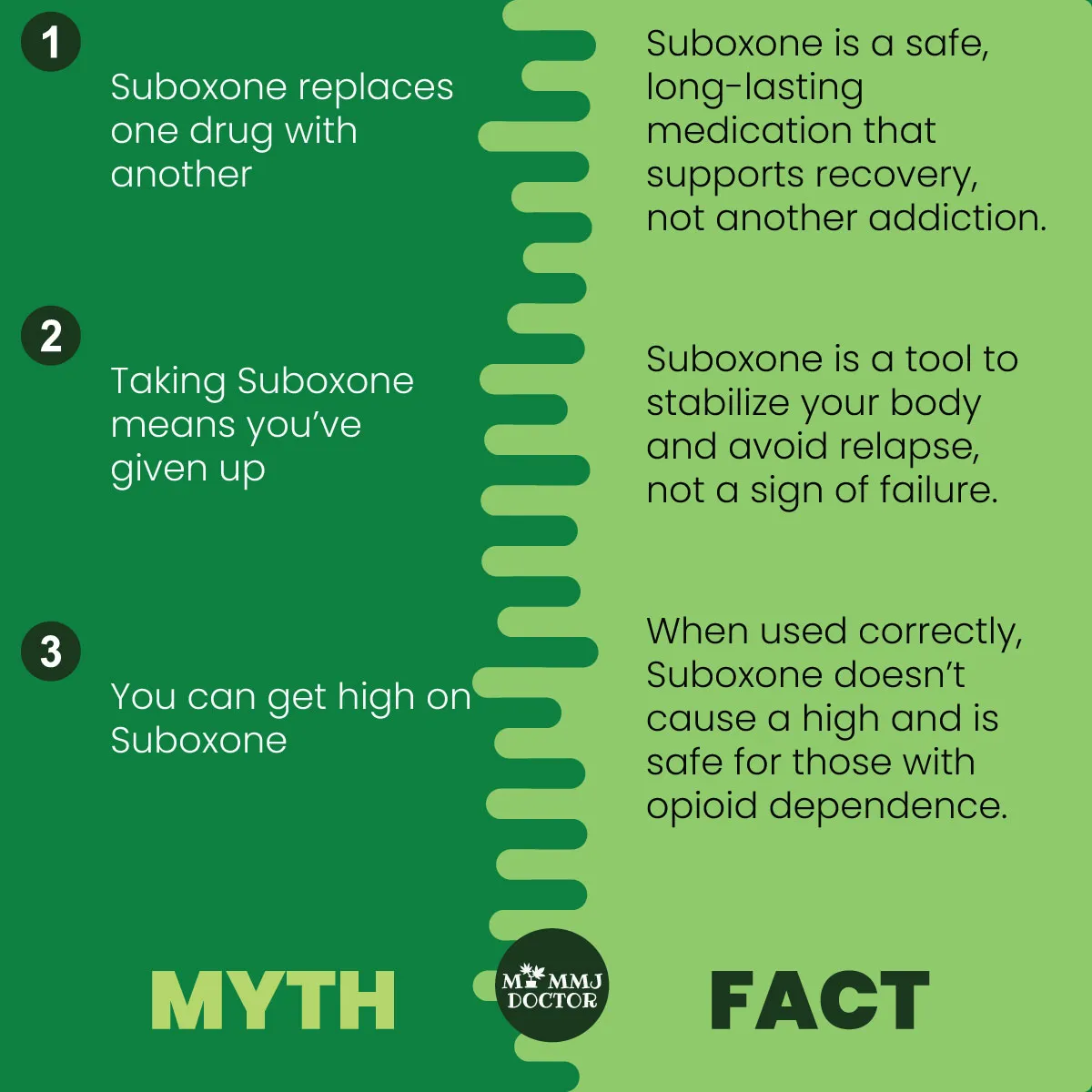
What are the misconceptions about Suboxone?
Misconception 1: Suboxone is just replacing one drug with another
Suboxone isn’t just switching one addiction for another. It’s a safe, long-lasting medication that helps improve your health, prevent diseases like HIV, and support recovery. It’s prescribed to treat addiction, not to cause another one.
Misconception 2: Taking Suboxone means you’ve given up
Addiction is a medical condition, not a lack of willpower. Suboxone helps stabilize your body so you can make positive changes and work towards recovery. It’s a tool to avoid dangerous relapses, not a sign of failure.
Misconception 3: You can get high on Suboxone
If used correctly by people with opioid dependence, Suboxone doesn’t cause a high. Misuse, such as combining it with other drugs or not following the prescription, can lead to problems, but patients using it properly are safe.
Suboxone vs Methadone:
| Suboxone | Methadone | |
|---|---|---|
| How it works | Combines buprenorphine (partial agonist) and naloxone; reduces cravings and prevents misuse. | Full opioid agonist; fully activates opioid receptors to reduce cravings and withdrawal. |
| Where it’s given | Often prescribed for home use, making it more accessible. | Administered at a clinic; requires regular visits. |
| Extra Uses | Mainly used to treat opioid addiction; not for pain or NAS. | Can treat babies born with opioid withdrawal (NAS) and chronic pain. |
| Risk | Lower overdose risk because of a “ceiling effect” with buprenorphine. | Higher risk of overdose due to its strength if taken improperly. |
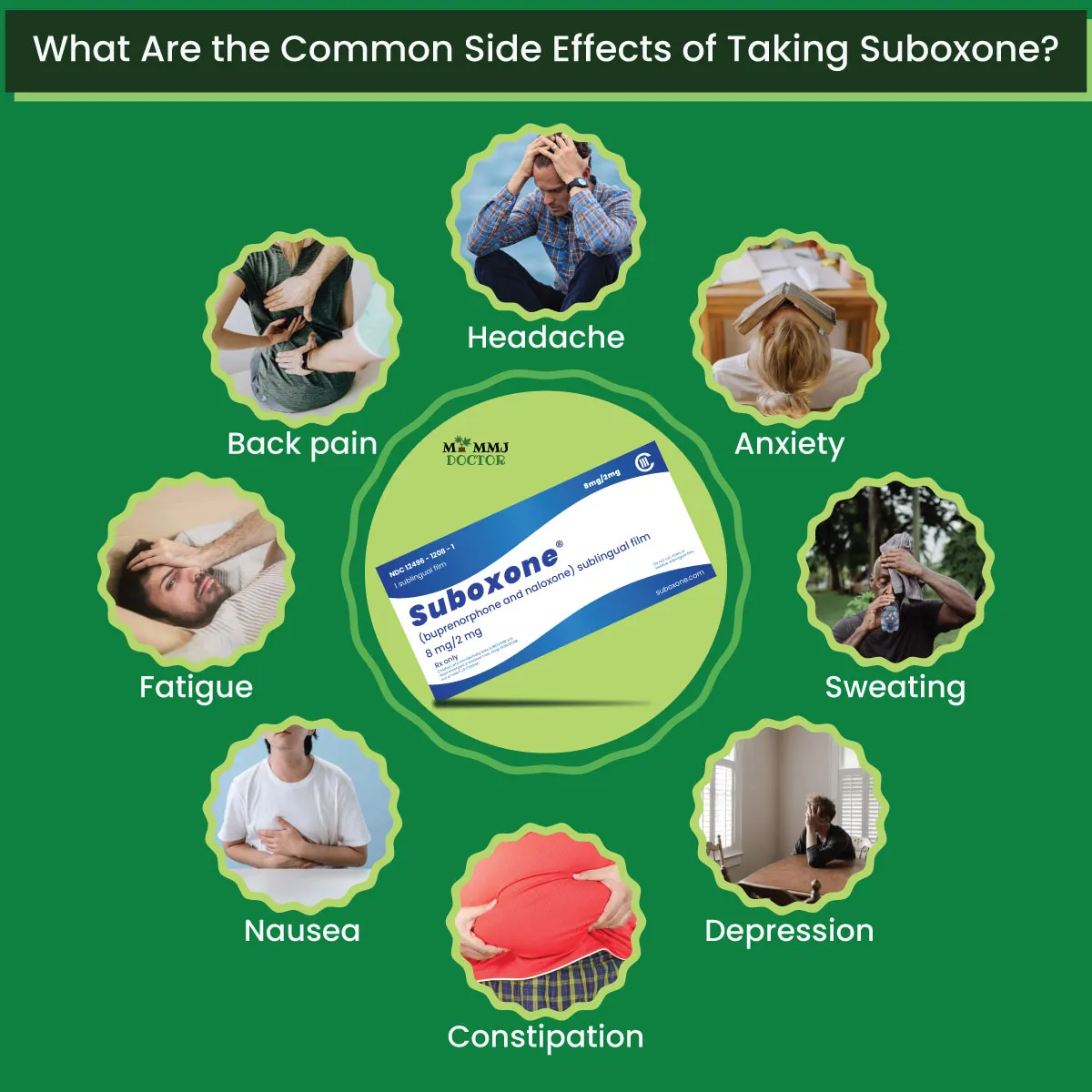
What are Suboxone Side-effects?
Common Side Effects:
- Headache
- Opioid withdrawal symptoms (body aches, cramps, fast heartbeat)
- Anxiety
- Insomnia (difficulty sleeping)
- Sweating
- Depression
- Constipation
- Nausea
- Fatigue or weakness
- Back pain
- Burning sensation in the mouth or tongue
- Redness in the mouth
Serious Side Effects:
Though rare, serious side effects can occur. Seek medical help immediately if you experience any of the following:
- Severe allergic reaction
- Misuse or dependence
- Breathing problems
- Coma
- Hormone issues (adrenal insufficiency)
- Liver damage
- Severe withdrawal symptoms
- Dental issues (cavities, tooth decay, infections)
Signs of a Severe Allergic Reaction:
- Difficulty breathing
- Skin rash or hives
- Swelling of lips, tongue, or throat
Conclusion
FAQs
- Does Suboxone help with pain?
Suboxone is not commonly used to treat pain. It is mainly prescribed for opioid addiction treatment, although buprenorphine, one of its components, can relieve pain at higher doses.
- Is Suboxone an opioid?
Yes, Suboxone contains buprenorphine, which is a partial opioid agonist. This means it acts on the brain’s opioid receptors but with a lower risk of abuse and overdose compared to full opioids.
- Can you overdose on Suboxone?
While it’s difficult to overdose on Suboxone due to its “ceiling effect” (it stops working more at higher doses), it’s still possible, especially if combined with other drugs like sedatives or alcohol.
- Does Suboxone show up on a drug test?
Suboxone can show up on specialized drug tests, but it typically won’t appear on standard drug screenings. However, certain tests can detect buprenorphine, one of its components.
- How Long Does Suboxone Stay in Your System?
The effects of Suboxone last around 24 hours in a healthy person. However, factors like your health and metabolism can affect how long it stays in your body.Suboxone’s half-life is 24 to 42 hours, meaning it takes that long for half of it to leave your system. For most people, it’s fully cleared from the body in 5 to 8 days and can be detected in drug tests during that time.
Related Articles
How Suboxone Works in Opioid Treatment?
How Suboxone Works in Opioid Treatment?Beating an addiction can be tough, especially when withdrawal symptoms make staying sober harder. Fortunately, Suboxone is a medication that can help ease these symptoms, allowing you to focus on...
How to Get Suboxone?
How to Get Suboxone?Opioid use disorder (OUD) is a public health issue that affects millions of individuals and their families. As the crisis gets worse, good treatment options are important for helping people take control of their lives. One...
How Long Should You Be on Suboxone?
How Long Should You Be on Suboxone?Some people may choose to take Suboxone for just a few months to manage withdrawal, while others may need it long-term to treat opioid use disorder (OUD). Suboxone helps reduce cravings, eases withdrawal...



0 Comments